Streamlining Healthcare Efficiency with Revenue Cycle Management (RCM)
Understanding Revenue Cycle Management (RCM)
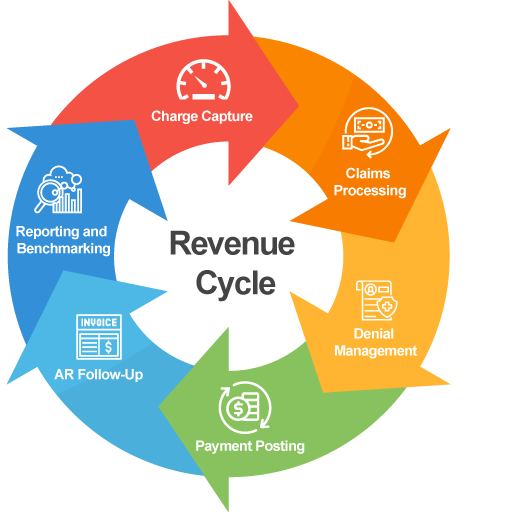
Revenue Cycle Management (RCM) plays a vital role in modern healthcare by managing the financial processes associated with patient care. It encompasses the entire lifecycle of a patient account, from initial appointment scheduling to the final payment of medical bills. RCM ensures that healthcare providers maintain a consistent and efficient cash flow while minimizing errors in billing and reimbursement.
In today’s increasingly complex medical environment, RCM serves as the backbone of healthcare operations. It bridges the gap between clinical care and financial sustainability by coordinating administrative and clinical functions such as coding, claim processing, and revenue collection. With the rise of electronic health records and automation tools, RCM systems have evolved into powerful platforms that enable organizations to focus on delivering quality care without being burdened by financial complications.
The Importance of RCM in Healthcare
Efficient Revenue Cycle Management directly impacts the financial health of medical practices and hospitals. It minimizes delays in claims processing and reduces denials through accurate data collection and error-free documentation. This streamlined process ensures that providers are reimbursed correctly and in a timely manner for services rendered.
Moreover, effective RCM enhances operational transparency and reduces administrative burdens. Healthcare organizations can monitor key performance indicators such as days in accounts receivable, denial rates, and collection percentages. These insights allow institutions to optimize workflows, lower overhead costs, and make data-driven decisions that support long-term growth and sustainability.
Core Components of Revenue Cycle Management
The revenue cycle begins with patient registration and insurance verification, which lays the foundation for successful claims submission. Accurate demographic and insurance data help prevent denials and ensure eligibility for coverage. Once care is provided, medical coding translates diagnoses and procedures into standardized codes for billing purposes.
Claims submission and payment posting follow, with systems verifying that payers process claims according to contractual agreements. In cases where claims are denied or underpaid, the RCM system enables quick resolution through appeals and follow-ups. Finally, patient billing and collections ensure that any remaining balances are communicated clearly and collected efficiently, closing the revenue loop.
Benefits of Implementing RCM Solutions
Adopting a comprehensive RCM solution offers significant advantages for healthcare providers. Automation reduces manual errors and administrative redundancies, accelerating the billing process and improving overall accuracy. This leads to faster reimbursements and lower rates of claim denials.
Additionally, RCM tools enhance patient satisfaction by offering transparent billing, flexible payment options, and better communication. When patients understand their financial responsibilities upfront and can easily access their billing information, they are more likely to complete payments on time, which in turn benefits the provider’s cash flow and service quality.
RCM and Regulatory Compliance
Healthcare providers must navigate an ever-changing landscape of regulations, including HIPAA, ICD-10, and payer-specific guidelines. RCM systems are designed to stay compliant with these standards, helping organizations avoid costly penalties and legal complications. By integrating updates and regulatory changes in real time, these platforms support ongoing compliance and reduce audit risks.
In addition, RCM promotes ethical billing practices and financial integrity. It fosters accountability through audit trails, data security measures, and standardized documentation. This level of compliance not only protects providers but also ensures that patients are treated fairly in all financial matters.
The Role of Technology in Modern RCM
Technological advancements have transformed RCM into a data-driven, intelligent process. Cloud-based platforms, artificial intelligence (AI), and machine learning algorithms are increasingly being used to automate claim edits, predict denials, and identify payment trends. These innovations reduce labor-intensive tasks and enable real-time decision-making.
Patient portals, automated reminders, and digital payment systems are also enhancing patient engagement and satisfaction. These tools provide convenience while minimizing delays and errors in communication. As a result, technology-driven RCM boosts overall efficiency, reduces costs, and strengthens the provider-patient relationship.
Challenges in Revenue Cycle Management
Despite its many benefits, RCM comes with challenges that require strategic planning and execution. Fragmented workflows, inaccurate coding, and insufficient training can all lead to claim denials and revenue loss. Moreover, shifting payer policies and frequent changes in reimbursement models can strain internal resources.
To overcome these challenges, healthcare providers must invest in continuous staff education, process optimization, and advanced analytics. Aligning clinical and financial teams also fosters a collaborative culture that enhances the revenue cycle's performance. Addressing these issues head-on helps maintain a robust and resilient RCM framework.
Improving RCM Through Best Practices
Implementing best practices is essential to maximizing the value of RCM. This includes verifying insurance eligibility in real time, consistently auditing claims for accuracy, and tracking denials to identify recurring issues. Clear communication with patients about their financial responsibilities is equally important for reducing billing disputes.
Moreover, regular staff training and leveraging RCM software for real-time performance insights can significantly enhance operational efficiency. Healthcare providers that prioritize continuous improvement in their revenue cycle are better positioned to deliver high-quality care while maintaining financial stability.
The Future of Revenue Cycle Management
The future of RCM lies in greater automation, enhanced interoperability, and patient-centric models. As healthcare transitions toward value-based care, RCM systems must adapt to support bundled payments, population health initiatives, and outcome-driven reimbursement models.
Artificial intelligence and predictive analytics will continue to refine billing accuracy and streamline denials management. Meanwhile, integration with electronic health records and payer systems will provide end-to-end visibility into patient encounters and payments. These advancements promise a more agile, responsive, and efficient revenue cycle ecosystem.
Source - https://www.marketresearchfuture.com/reports/revenue-cycle-management-market-18856
Revenue Cycle Management is a cornerstone of financial success and patient satisfaction in healthcare. By streamlining the administrative and billing processes, RCM allows providers to focus on delivering quality care while ensuring timely and accurate reimbursements. With evolving technology and industry demands, RCM will continue to be a strategic priority for healthcare organizations aiming to thrive in an increasingly complex environment.
- Art
- Causes
- Crafts
- Dance
- Drinks
- Film
- Fitness
- Food
- Games
- Gardening
- Health
- Home
- Literature
- Music
- Networking
- Other
- Party
- Religion
- Shopping
- Sports
- Theater
- Wellness